Temporomandibular Disorders (TMD)
Published on
18 Sep 2017

Call us on: (03) 9975 4133
The temporomandibular joint (TMJ) is a part of the body you may not know much about. We hear a lot about other injuries, back, hip, knee, shoulder, and so on but how often do we hear about jaw pain? In fact studies show that around 16% of the population need treatment for jaw pain. You, or someone you know, may be experiencing it. So who do you go to see? Your doctor? A dentist? Did you know that physiotherapists can treat jaw pain? Let’s explain a little about some of the anatomy and you’ll see why a physio might be the best person to see.
Anatomy
The jaw is comprised of some basic anatomy similar to other joints; bone, cartilage, disc, muscles, and tendons.
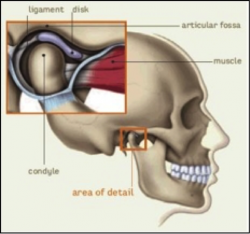
The mandibular condyle sits in the articular fossa of the skull. Each surface is covered with cartilage and the joint is reinforced by a joint capsule and ligaments. Within the joint is a disc, which allows smooth opening and closing of the mouth.
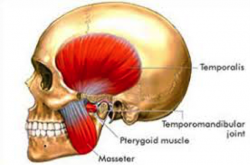
The primary muscles involved at the TMJ are:
- temporalis
- masseter
- medial and lateral pterygoids
Disorders
TMD can be divided into two categories:
1) symptoms originating from the joint, or;
2) symptoms originating from the muscles.
Typically however there is overlap between these two areas. Problems may come about suddenly such as with trauma like a fractures or whiplash, or may be a gradual onset over time.
Symptoms can include,
- pain locally at the joint or referred into the neck, head, face or teeth
- noises such as clicking, popping, grinding
- limited range of movement, which may cause difficulties with eating, yawning, singing, etc.
- asymmetrical movement pattern. The jaw may deviate to one side or the other, or may do an ‘S’ movement on opening
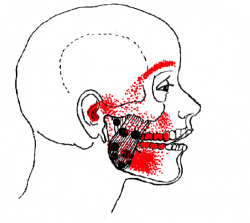
Pictured: Areas of possible referred pain from muscles around the TMJ.
What else contributes to TMD?
Cervical (neck) posture has an influence on TMJ mechanics. If you are hunched over a computer for extended periods, not only will your neck and upper back be subject to tension, your jaw will be too. Try this experiment – sit upright with good posture and clench your teeth. Notice the bite pattern. Now slouch. Let your head sink forwards and your upper back round. Bite again. Is the bite pattern the same? Or do you notice a difference?
Stress, clenching or grinding will also add load to the joint over time. Do you notice if your teeth touch during the day? Or do you know that you grind your teeth in the night (bruxism)? Perhaps your dentist has noticed the effects of grinding on your teeth? If you are aware of bruxism or related problems on your teeth, speak with your dentist about a night splint to protect your teeth.
If you know you clench your teeth during the day, focus on relaxing the jaw. A resting position for your jaw should be with the teeth apart and the tongue resting on the roof of the mouth as if saying a soft ‘n’. If stress is an issue for you, practice some relaxation techniques or speak with a professional about additional stress relieving strategies.
What physiotherapy can offer?
A full assessment will be done to ascertain where the symptoms originate and what the main problems are. Treatment will then be carried accordingly and can include,
- Mobilisations to the joint to increase range of movement and reduce pain
- Local muscle release to reduce tension and/or trigger points
- Cervical spine treatment, if contributing to the jaw pain
- Exercises to improve range, reduce muscle tension, and improve resting position
- Liaise with your dentist for splints or dental work; your GP for pain relief medication; or other professional for stress management
We’re Here to Help!
So if you are experiencing any symptoms associated with TMD, make sure you see your physiotherapist as a first port of call. Don’t suffer in silence – contact us today!


